DRC © 2024 MSF
Mpox
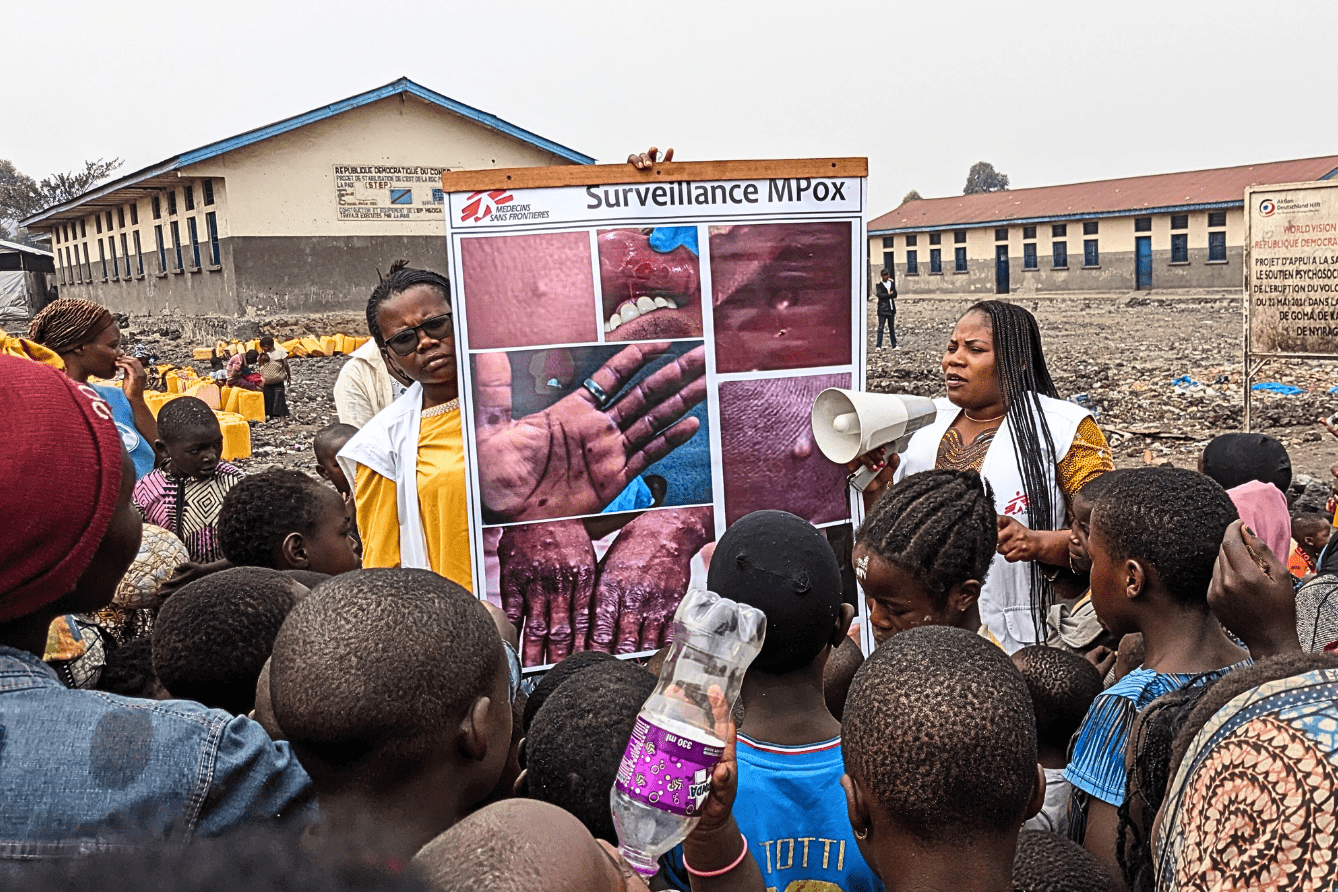
Mpox, formerly known as monkeypox, is a contagious viral disease that can be especially serious for children, pregnant women, and people with weakened immune systems. Increased access to vaccines is critical to prevent its spread.
Mpox outbreak in DR Congo: What to know
August 15, 2024 — The mpox epidemic currently sweeping through Democratic Republic of Congo (DRC) is spreading at an alarming rate—and has been reported beyond the country’s borders. Between January and the beginning of August, more than 14,000 suspected cases were reported in 23 affected provinces in DRC, as a genetic mutation has been causing uninterrupted human-to-human transmission of the virus for months.
Read more
Putting mpox in context
Mpox, previously known as monkeypox, is a contagious viral disease that can cause skin lesions, fever, headache, muscle aches, exhaustion, and swollen lymph nodes. Its symptoms are usually mild and last from two to four weeks, but more severe cases can occur. Those most vulnerable to severe forms of the disease include children, pregnant women, and people with weakened immune systems.
Mpox cases have been on the rise in Democratic Republic of the Congo (DRC) for more than two years, and the situation has worsened in recent months. As the virus has mutated, leading to human-to human transmission, there has been a surge in the number of people infected and suspected cases in camps for displaced people.
On August 14, 2024, the World Health Organization director-general declared that the surge of mpox cases in DRC and a growing number of countries in Africa constitutes a public health emergency of international concern. The emergency declaration followed advice from an expert committee warning that the disease has the potential to spread further across countries in Africa and possibly outside the continent.
MSF teams have set up several interventions to support the response to the outbreak in DRC, initially focused in South Kivu and North Kivu.
The first case of mpox in a human was identified in DRC in 1970. Today, the disease is endemic in 11 countries in West and Central Africa. However, there have been some outbreaks outside of the continent in people who were exposed during travel or through imported animals that had the virus. In 2022, an unprecedented outbreak of cases spread in countries across the world that do not normally report mpox, with the largest number of confirmed cases reported in the US.
Facts about mpox
Mpox is in the same class of viruses as smallpox, which had similar but more severe symptoms before its eradication in the late 1970s.
The mpox virus is primarily spread through close human-to-human contact, including in the respiratory droplets and contact with skin lesions of someone who has the disease. The virus can enter a person’s body through broken skin, the respiratory tract, and the eyes, nose, mouth, or through sexual contact. In order for the virus to spread through respiratory droplets, a person has to be face-to-face with someone who is sick for a prolonged period—putting health workers and family members at the greatest risk of contracting the virus from someone who has it. It can also be spread by touching objects like clothes or furniture that have the virus on them.
The current outbreak has disproportionately affected men who have sex with men, but anyone can become infected if exposed to the virus.
While the most common symptoms of mpox are skin lesions, fever, headache, muscle aches, exhaustion, and swollen lymph nodes, complications have been reported, primarily among people with other health conditions. These include secondary infections, bronchopneumonia, sepsis, encephalitis, and infection of the cornea and subsequent loss of vision.
Most people who are infected with mpox recover from their symptoms within four weeks. The percentage of people who die from mpox compared to the number of those infected has historically been 3-6 percent in places where the disease is endemic. The reported death rate in the 2022 outbreak—in which the majority of cases have been reported in the US and Europe—is significantly lower than this.
The severity of one’s illness is also dependent on which strain of the virus they contract. There are two main strains of mpox, the Clade I and Clade II strains. The Clade II strain of mpox causes less severe disease compared to the Clade I strain of the disease, with case fatality rates of 3.6 percent and 10.6 percent, respectively.
The most effective test for mpox is a real-time polymerase chain reaction (RT-PCR) test that takes a sample from a person’s infected skin lesion. There are currently no over-the-counter diagnostic tests available.
Two antiviral medicines—tecovirimat and brincidofovir—were recently approved for poxviruses, including smallpox and mpox, in the US and/or Europe.
Prevention is also key in curbing the spread of mpox. People should avoid close contact with those who have mpox or an mpox-like rash, avoid touching objects that have been used by people with the virus, and wash their hands often.
Data from studies conducted in Africa show that the smallpox vaccine may be up to 85 percent effective in preventing mpox infection. However, since smallpox was eradicated and vaccine campaigns against it have ended, fewer people across the world have existing immunity.
Currently, more than 116 million doses of smallpox vaccine are scattered among various national stockpiles as part of biodefence strategies against smallpox, with the US holding the vast majority. The US is currently stockpiling more than 100 million doses of a smallpox vaccine called ACAM2000. However, this vaccine can cause significant side effects and adverse events. The preferred vaccine to protect against mpox is JYNNEOS, but supply of this vaccine is much more limited, especially in countries where mpox is endemic.
In order to protect people who are most at risk of contracting mpox, it is critical that vaccines are widely accessible and affordable and that wealthy countries do not hoard them as has been seen during the COVID-19 pandemic. It is especially important to ensure access to vaccines for people living in the places that have historically seen the most mpox cases, including countries in West and Central Africa.

More news and stories
Learn about MSF’s journalistic roots and our commitment to bear witness and speak out about the plight of the people we treat.
Learn about MSF’s journalistic roots and our commitment to bear witness and speak out about the plight of the people we treat.






